ER Nurse vs. ICU Nurse: What’s the Difference?
In the dynamic landscape of modern healthcare, the demand for highly skilled nurses capable of handling high-stakes situations has never been greater. Emergency Room (ER) nursing and Intensive Care Unit (ICU) nursing are among the most demanding and rewarding nursing specialities. Both roles operate at the sharp end of patient care, dealing with critical conditions and making life-saving decisions.
However, despite some overlap in the acuity of patients they see, the day-to-day realities, required skill sets, and work environments differ significantly. Many nursing students, new graduates, and even experienced RNs debate: ER or ICU? Understanding the core distinctions is crucial for making an informed career choice that aligns with your strengths, personality, and professional aspirations. This article provides a comprehensive, side-by-side comparison of the **ER nurse vs ICU nurse** roles to illuminate the unique challenges and rewards of each path.
Section 1: Overview of Each Role
What Does an ER Nurse Do?
An Emergency Room (ER) Nurse, also known as an Emergency Department (ED) Nurse, is a registered nurse (RN) specializing in rapid assessment and treatment of patients experiencing acute illnesses or injuries. They are the front line of emergency medical care within a hospital setting. Its unpredictable nature characterizes the ER; nurses must be prepared to handle anything from minor ailments to life-threatening trauma without prior notice.
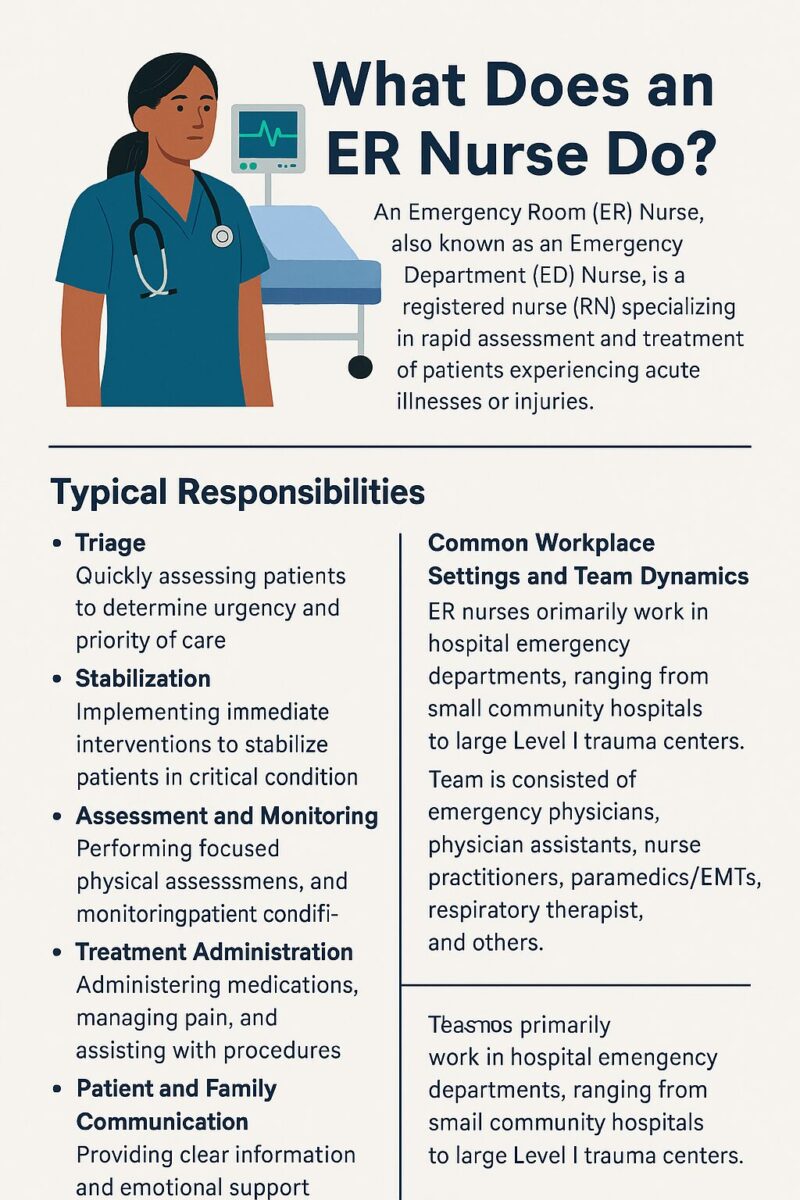
Typical Responsibilities:
- Triage: Quickly assessing patients upon arrival to determine the urgency and priority of care based on established protocols (e.g., Emergency Severity Index – ESI).
- Stabilization: Implementing immediate interventions to stabilize patients in critical condition (e.g., administering oxygen, starting IV lines, performing CPR, assisting with intubation).
- Assessment and Monitoring: Performing focused physical assessments, obtaining vital signs, and monitoring patient conditions for rapid changes.
- Treatment Administration: Administering medications (including emergency drugs), managing pain, dressing wounds, and assisting physicians with procedures (e.g., suturing, casting, chest tube insertion).
- Patient and Family Communication: Providing clear information and emotional support to patients and their families during stressful situations.
- Documentation: Accurately and efficiently charting assessments, interventions, and patient responses in the electronic health record (EHR).
- Coordination of Care: Collaborating with physicians, specialists, technicians, and ancillary staff; facilitating patient transfers to inpatient units (like the ICU) or discharge home.
Common Workplace Settings and Team Dynamics: ER nurses primarily work in hospital emergency departments, ranging from small community hospitals to large Level I trauma centers. The team is typically large and diverse, including emergency physicians, physician assistants, nurse practitioners, paramedics/EMTs (bringing patients in), respiratory therapists, radiology technicians, pharmacists, social workers, and patient care technicians. The environment is fast-paced, often loud, and requires seamless teamwork and communication under pressure.
The **ER nurse job description** emphasizes adaptability, quick thinking, and the ability to manage multiple patients with diverse conditions simultaneously.
What Does an ICU Nurse Do?
An Intensive Care Unit (ICU) Nurse, often called a Critical Care Nurse, is an RN specializing in the care of patients with life-threatening conditions requiring complex assessment, high-intensity therapies, and continuous monitoring. Unlike the rapid turnover in the ER, ICU nurses often manage one or two patients for extended periods, allowing for in-depth care and relationship building.
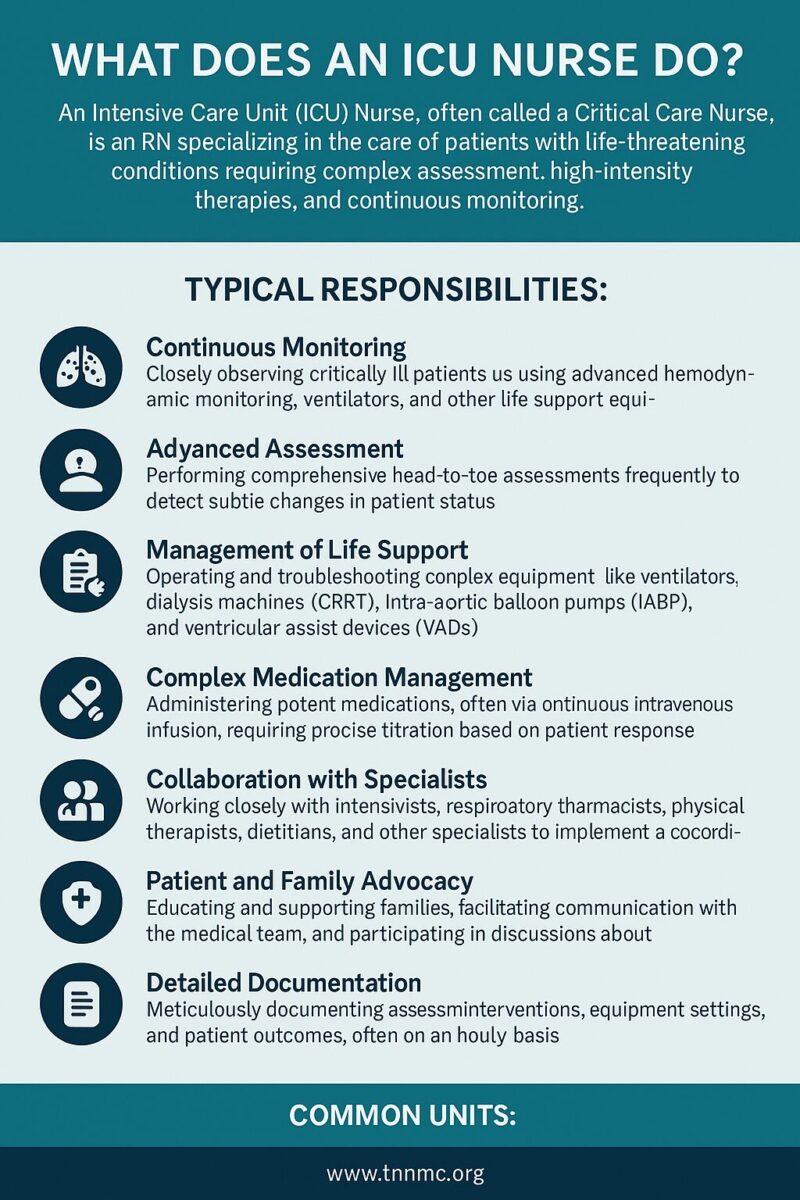
Typical Responsibilities:
- Continuous Monitoring: Closely observing critically ill patients using advanced hemodynamic monitoring, ventilators, and other life support equipment. Interpreting complex data streams (e.g., ECG rhythms, arterial blood pressure, ventilator settings).
- Advanced Assessment: Performing comprehensive head-to-toe assessments frequently to detect subtle changes in patient status.
- Management of Life Support: Operating and troubleshooting complex equipment like ventilators, dialysis machines (CRRT), intra-aortic balloon pumps (IABP), and ventricular assist devices (VADs).
- Complex Medication Management: Administering potent medications, often via continuous intravenous infusion (e.g., vasopressors, sedatives, paralytics), requiring precise titration based on patient response.
- Collaboration with Specialists: Working closely with intensivists (physicians specializing in critical care), respiratory therapists, pharmacists, physical therapists, dietitians, and other specialists to implement a coordinated plan of care.
- Patient and Family Advocacy: Educating and supporting families, facilitating communication with the medical team, and participating in discussions about goals of care and end-of-life decisions.
- Detailed Documentation: Meticulously documenting assessments, interventions, equipment settings, and patient outcomes, often on an hourly basis.
Common Units: ICUs are often specialized based on patient populations. Common types include:
- Medical ICU (MICU): Patients with severe medical conditions like sepsis, respiratory failure, or diabetic ketoacidosis.
- Surgical ICU (SICU): Patients recovering from major surgeries or trauma.
- Cardiac ICU (CICU) or Cardiovascular ICU (CVICU): Patients with acute heart conditions, post-cardiac surgery.
- Neurological ICU (Neuro ICU): Patients with critical neurological conditions like stroke, brain injury, or seizures.
- Pediatric ICU (PICU) and Neonatal ICU (NICU): Specialized units for critically ill children and newborns.
The **ICU nurse responsibilities** revolve around vigilance, meticulous attention to detail, deep physiological knowledge, and the ability to manage complex technologies and therapies over sustained periods.
Section 2: Key Differences Between ER Nurses and ICU Nurses
While both ER and ICU nurses care for critically ill patients, the fundamental **difference between ER and ICU nurse** roles lies in the context, pace, and focus of their work.
Work Environment and Patient Interaction
- ER: A dynamic, high-traffic environment focused on rapid assessment, stabilization, and disposition (admission, transfer, or discharge). Patient interactions are typically short-term and episodic. Nurses manage a higher volume of patients with a wide spectrum of acuities, often seeing many patients per shift. The primary goal is to identify life threats, stabilize, and move the patient to the next appropriate level of care quickly.
- ICU: A more controlled, though intense, environment focused on in-depth, continuous care for a small number of critically ill patients (usually a 1:1 or 1:2 nurse-to-patient ratio). Patient interactions are prolonged, often spanning days or weeks. Nurses develop a deep understanding of their specific patients’ complex conditions and provide comprehensive management aimed at recovery or stabilization over time.
Pace and Work Style
- ER: Extremely fast-paced, characterized by frequent interruptions, context switching, and the need to constantly re-prioritize based on new arrivals and changing patient conditions. Requires exceptional multitasking skills and the ability to thrive in controlled chaos. Decision-making is often rapid, based on focused assessments and protocols.
- ICU: A pace that is often described as intensely focused rather than chaotic. While emergencies (like codes or rapid declines) occur, much of the work involves meticulous monitoring, planned interventions, and detailed analysis of trends. Requires a methodical, detail-oriented approach and sustained concentration. Decision-making is often collaborative and based on in-depth data analysis.
Typical Patient Cases
- ER: A broad mix of everything imaginable, often undiagnosed on arrival. Common cases include:
- Trauma (from minor injuries to multi-system trauma)
- Stroke (requiring rapid identification for time-sensitive treatment)
- Heart Attack (STEMI/NSTEMI)
- Sepsis (early identification and resuscitation)
- Respiratory distress (asthma, COPD exacerbation, pneumonia)
- Overdoses and poisonings
- Severe allergic reactions (anaphylaxis)
- Acute abdominal pain
- Psychiatric emergencies
- Minor illnesses and injuries
- ICU: Patients who are already diagnosed (often from the ER or OR) and require intensive support. Common cases include:
- Severe Sepsis / Septic Shock
- Acute Respiratory Distress Syndrome (ARDS) requiring mechanical ventilation
- Multi-organ failure
- Complex post-operative recovery (e.g., open-heart surgery, organ transplant, major abdominal surgery)
- Traumatic Brain Injury (TBI) or Spinal Cord Injury
- Severe stroke requiring intensive monitoring
- Cardiogenic shock requiring mechanical circulatory support (IABP, VAD)
- Continuous Renal Replacement Therapy (CRRT) for kidney failure
Required Skills and Mindset
Both roles demand exceptional critical thinking, clinical judgment, and technical skills. However, the emphasis differs:
- ER Nurse:
- Strengths: Rapid assessment, expert triage, procedural skills (IV starts, catheter insertion, wound care), crisis management, adaptability, broad knowledge base across many conditions, quick decision-making under pressure, excellent time management and prioritization, thrives on unpredictability.
- Mindset: Action-oriented, comfortable with ambiguity, high tolerance for chaos, skilled at quickly establishing rapport, decisive.
- ICU Nurse:
- Strengths: In-depth physiological understanding, advanced assessment skills, expertise in managing complex equipment (vents, drips, monitors), meticulous attention to detail, anticipates complications, strong analytical skills, excels at interpreting subtle trends, manages long-term critical care plans.
- Mindset: Detail-oriented, analytical, proactive, patient, high tolerance for sustained intensity, skilled at deep dives into pathophysiology, comfortable with complex technology.
This comparison of **critical care nurse vs emergency nurse** highlights the different types of intensity and focus required.
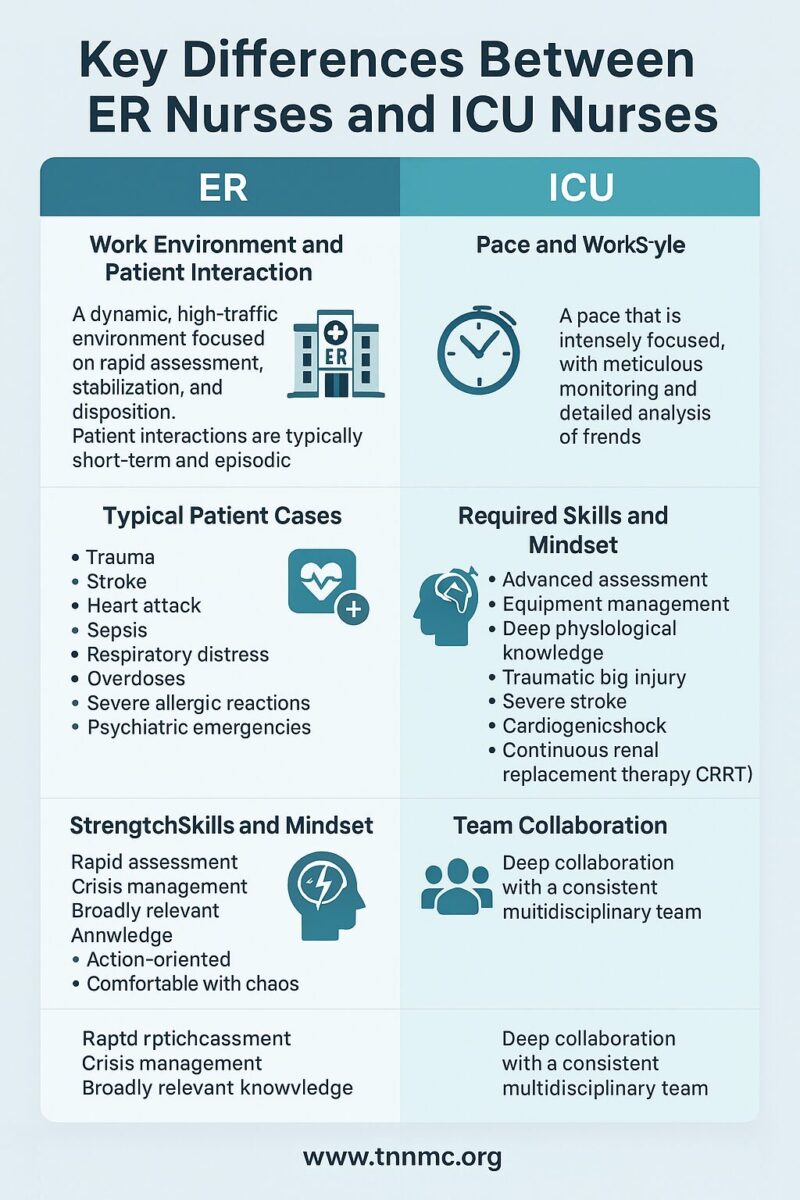
Team Collaboration
- ER: Involves broad collaboration with a constantly changing team and external partners. Key interactions include EMS personnel during patient handoffs, rapid response teams, various physician specialists called for consults, radiology, lab, and social work. Communication needs to be concise and efficient to facilitate rapid patient flow.
- ICU: Characterized by deep collaboration within a more consistent multidisciplinary team focused on specific patients. Daily rounds involving intensivists, pharmacists, respiratory therapists, dietitians, and sometimes physical/occupational therapists are common. Communication is detailed and focused on comprehensive care planning and adjustments.
Section 3: Education, Certification & Career Pathways
Education Requirements
A Registered Nurse (RN) license is the minimum requirement to become an ER or ICU nurse. This typically requires completing either:
- An Associate Degree in Nursing (ADN) – Usually a 2-year program.
- A Bachelor of Science in Nursing (BSN) – Typically a 4-year program.
After graduating from an accredited nursing program, candidates must pass the National Council Licensure Examination (NCLEX-RN) to obtain their RN license.
Emphasis on BSN: While an ADN allows entry into practice, there is a strong and growing preference among employers, particularly magnet hospitals and those hiring for specialty areas like the ICU and ER, for nurses with a BSN degree. Research suggests BSN-prepared nurses are associated with better patient outcomes. The Institute of Medicine (now the National Academy of Medicine) has recommended increasing the proportion of BSN-prepared nurses in the workforce. Many healthcare organizations offer tuition assistance for ADN nurses to pursue BSN completion programs (RN-to-BSN).
Certifications
While not always mandatory initially, specialty certifications are highly recommended and often required for advancement or specialized roles within the ER and ICU. They demonstrate advanced knowledge and commitment to the specialty.
- ER Nurse: The primary certification is the Certified Emergency Nurse (CEN), offered by the Board of Certification for Emergency Nursing (BCEN). Eligibility typically requires an active RN license and recommended experience (often 2 years) in the ER setting.
- ICU Nurse: The most recognized certification is the Critical Care Registered Nurse (CCRN), offered by the American Association of Critical-Care Nurses (AACN). There are variations for adult, pediatric, and neonatal critical care. Eligibility requires specific clinical practice hour requirements in critical care.
Other Important Certifications (Often Required by Employers):
- Basic Life Support (BLS): Required for all nurses.
- Advanced Cardiovascular Life Support (ACLS): Essential for both ER and ICU nurses dealing with adult cardiac emergencies.
- Pediatric Advanced Life Support (PALS): Required for nurses working in ERs or ICUs that treat children.
- Trauma Nursing Core Course (TNCC): Highly valued for ER nurses, especially in trauma centers, and beneficial for SICU nurses. Offered by the Emergency Nurses Association (ENA).
- Emergency Nursing Pediatric Course (ENPC): Similar to PALS but focused specifically on the emergency nursing care of children, also offered by the ENA.
You can find more information at the websites for the Emergency Nurses Association (ENA) and the American Association of Critical-Care Nurses (AACN).
Recommended Experience or Training
Most hospitals prefer or require some level of general nursing experience (e.g., on a medical-surgical floor) before transitioning into the high-acuity environments of the ER or ICU, although some offer new graduate residency programs for these specialties.
- For ER: Experience in settings that require quick assessment and intervention skills (like telemetry or step-down units) can be beneficial. Training often focuses on triage systems, trauma care protocols, managing diverse patient populations rapidly, and mastering common ER procedures.
- For ICU: Experience on telemetry or progressive care units (PCU)/step-down units is a common pathway. Training emphasizes advanced hemodynamics, ventilator management, interpreting complex monitoring data, managing critical medication drips, and understanding specific critical care disease processes.
Advancement Opportunities
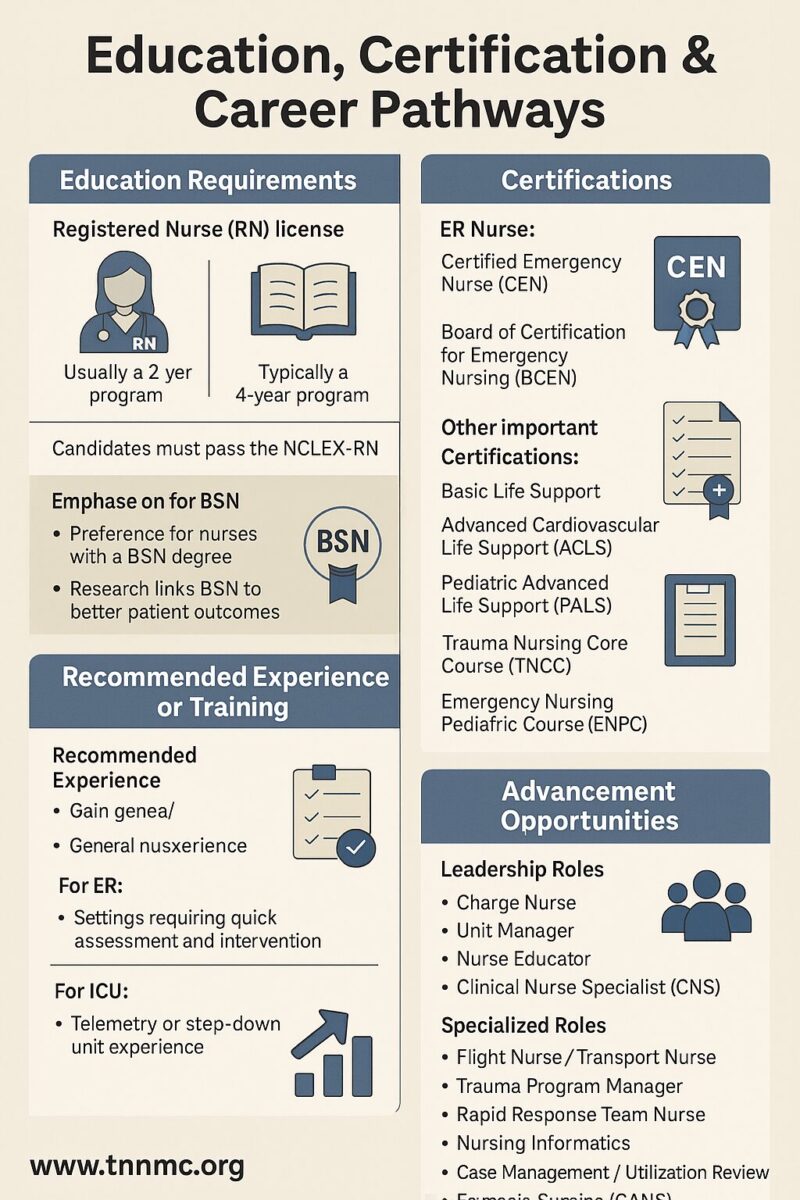
Both ER and ICU nursing offer numerous pathways for career growth:
- Leadership Roles: Charge Nurse, Unit Manager, Nurse Educator, Clinical Nurse Specialist (CNS).
- Advanced Practice Registered Nurse (APRN):
- Nurse Practitioner (NP): Acute Care NP (ACNP) is common for ICU backgrounds; Emergency NP (ENP) or Family NP (FNP) with emergency experience for ER backgrounds.
- Certified Registered Nurse Anesthetist (CRNA): Requires critical care experience (ICU is often preferred or required).
- Specialized Roles:
- Flight Nurse / Transport Nurse: Often requires extensive ER and/or ICU experience and additional certifications.
- Trauma Program Manager: Typically requires strong ER/Trauma experience.
- Rapid Response Team Nurse: Often staffed by experienced ICU or ER nurses.
- Nursing Informatics: Leveraging clinical experience to improve EHRs and clinical technology.
- Case Management / Utilization Review: Roles focusing on care coordination and resource management.
- Forensic Nursing (SANE): Often based in the ER.
This diverse range of options underscores the value of experience gained in these demanding specialties.
Section 4: Salary and Job Outlook
Both ER and ICU nursing are in-demand specialties with competitive salaries, reflecting the high level of skill and stress involved. Salary can vary significantly based on geographic location, years of experience, education level (BSN often commands higher pay), certifications, unionization, and the specific healthcare facility.
ER Nurse vs. ICU Nurse Salary Comparison
Obtaining precise, real-time salary figures is challenging as data comes from various sources with different methodologies and reporting dates. The following table provides estimated ranges and factors based on recent data from sources like the U.S. Bureau of Labor Statistics (BLS), Medscape, Salary.com, Nurse.org, and ZipRecruiter (as of late 2024 / early 2025 – *Note: Always check current sources for the most up-to-date figures*).
| Role | Estimated Average Annual Salary Range (US) | Common High-Paying States/Metro Areas | Key Certifications Influencing Pay | General Job Outlook |
|---|---|---|---|---|
| ER Nurse | $78,000 – $105,000+ | California, Hawaii, Oregon, Washington, Massachusetts, Alaska, New York City, Washington D.C. | CEN, TNCC, ACLS, PALS, ENPC | Strong / Growing |
| ICU Nurse | $82,000 – $115,000+ | California, Hawaii, Oregon, Washington, Massachusetts, Alaska, New York, Washington D.C. | CCRN, ACLS, TNCC (esp. SICU) | Very Strong / High Demand |
Important Salary Considerations:
- ICU tends to pay slightly higher on average: This often reflects the specialized knowledge required for managing complex equipment and long-term critical patients, along with the high demand for CCRN-certified nurses. The **ICU vs emergency nurse salary** difference is usually modest but present in many markets.
- Location is a Major Factor: Salaries are significantly higher in states with a high cost of living and strong nursing unions (e.g., West Coast, Northeast).
- Experience Matters: Pay increases substantially with years of experience in the specialty.
- Certifications Boost Earnings: Holding specialty certifications like CEN or CCRN often leads to higher pay rates or clinical ladder advancements.
- Overtime and Differentials: Actual earnings can be much higher due to shift differentials (nights, weekends), overtime opportunities, and potential charge nurse or preceptor pay.
Job Outlook
The overall job outlook for Registered Nurses is excellent. The U.S. Bureau of Labor Statistics (BLS) projects employment for RNs to grow faster than the average for all occupations through the next decade (check the BLS Occupational Outlook Handbook for the latest projection).
Within nursing, the demand for both ER and ICU nurses is particularly strong due to:
- Aging Population: An increasing number of older adults with complex, chronic, and acute health conditions require emergency and critical care services.
- Advancements in Medicine: Medical technology allows for more complex interventions and supports critically ill patients for longer durations, increasing the need for skilled ICU nurses.
- Increased Hospital Acuity: Hospitals increasingly care for sicker patients, concentrating those needing high-level monitoring and intervention in ICU and ER settings.
- Nurse Shortages: Ongoing shortages in specialized areas like critical care and emergency nursing create numerous job openings across the country.
Both fields offer significant job security and opportunities for employment nationwide.

Section 5: Which Role Is Right for You?
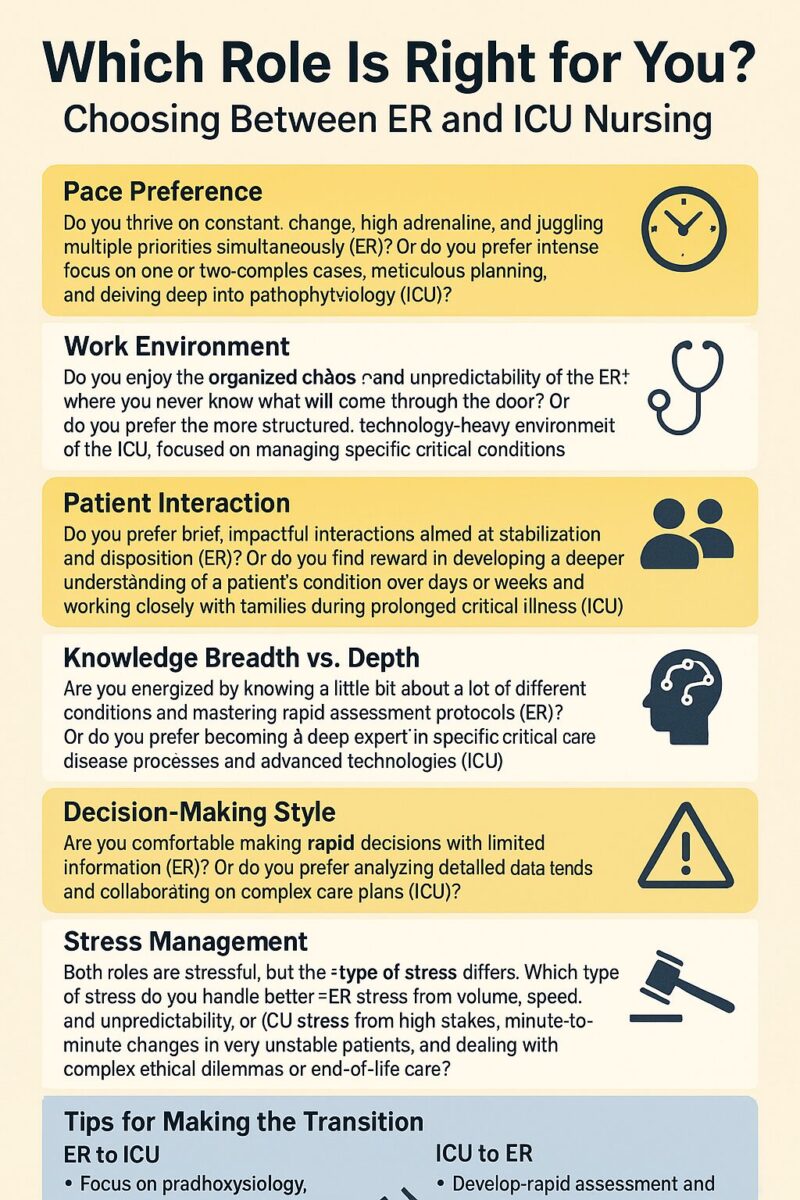
Choosing Between ER and ICU Nursing
Deciding between the ER and the ICU depends heavily on your personality, preferred work style, and long-term career goals. There’s no single “better” choice; it’s about finding the best fit. Ask yourself:
- Pace Preference: Do you thrive on constant change, high adrenaline, and juggling multiple priorities simultaneously (ER)? Or do you prefer intense focus on one or two complex cases, meticulous planning, and delving deep into pathophysiology (ICU)?
- Work Environment: Do you enjoy the organized chaos and unpredictability of the ER, where you never know what will come through the door? Or do you prefer the more structured, technology-heavy environment of the ICU, focused on managing specific critical conditions?
- Patient Interaction: Do you prefer brief, impactful interactions aimed at stabilization and disposition (ER)? Or do you find reward in developing a deeper understanding of a patient’s condition over days or weeks and working closely with families during prolonged critical illness (ICU)?
- Knowledge Breadth vs. Depth: Are you energized by knowing a little bit about a lot of different conditions and mastering rapid assessment protocols (ER)? Or do you prefer becoming a deep expert in specific critical care disease processes and advanced technologies (ICU)?
- Decision-Making Style: Are you comfortable making rapid decisions with limited information (ER)? Or do you prefer analyzing detailed data trends and collaborating on complex care plans (ICU)?
- Stress Management: Both roles are stressful, but the *type* of stress differs. ER stress often comes from volume, speed, and unpredictability. ICU stress often relates to the high stakes of managing minute-to-minute changes in very unstable patients and dealing with complex ethical dilemmas or end-of-life care. Which type of stress do you handle better?
Considering **which is better ER or ICU nurse** for *you* requires honest self-reflection on these points.
Tips for Making the Transition
It’s possible, though challenging, to transition between these specialties. Skills learned in one area are often valuable in the other.
- ER to ICU: Focus on deepening your understanding of pathophysiology, ventilator management, hemodynamic monitoring, and managing critical drips. Consider taking critical care courses or seeking experience on a step-down unit (PCU). Shadowing ICU nurses is invaluable. Emphasize your assessment skills and ability to handle emergencies.
- ICU to ER: Focus on developing rapid assessment and triage skills, managing patient flow, and broadening your knowledge base to handle a wider variety of conditions (including lower acuity cases). Practice multitasking and quick decision-making. Highlight your strong assessment skills, understanding of critical conditions, and calmness under pressure. Shadowing ER nurses is crucial.
- Gaining Dual Experience: Some nurses work per diem or float between departments (if hospital policy allows) to gain exposure to both environments. This can make you a highly versatile and marketable nurse.
Conclusion
Both Emergency Room (ER) and Intensive Care Unit (ICU) nursing represent challenging, vital, and rewarding career paths within the nursing profession. ER nurses excel in fast-paced, unpredictable environments, mastering rapid assessment, stabilization, and managing a high volume of diverse cases. ICU nurses thrive on deep, focused care for the most critically ill, mastering complex technologies and providing meticulous, long-term monitoring and intervention. The **difference between ER and ICU nurse** roles is significant in terms of pace, environment, patient interaction, and specific skill emphasis.
Choosing between them depends on your individual personality, strengths, and career aspirations. Both specialties offer strong job security, competitive salaries (with **ICU vs emergency nurse salary** often slightly favoring ICU), and numerous opportunities for professional growth and advancement. Whether you’re drawn to the controlled chaos of the ER or the focused intensity of the ICU, pursuing further education (like a BSN) and specialty certifications (CEN or CCRN) will enhance your skills, marketability, and earning potential.
Reflect on what energizes you, the type of patient care you find most fulfilling, and the work environment where you believe you’ll thrive. Both ER and ICU nurses make a profound difference in the lives of patients and families during their most vulnerable moments.
Sources & References (Examples – link to specific pages where possible)
- U.S. Bureau of Labor Statistics (BLS): Occupational Outlook Handbook – Registered Nurses
- American Association of Critical-Care Nurses (AACN): www.aacn.org (Information on CCRN certification, critical care practice)
- Emergency Nurses Association (ENA): www.ena.org (Information on CEN certification, TNCC, ENPC, emergency nursing practice)
- Board of Certification for Emergency Nursing (BCEN): bcen.org
- Salary Comparison Websites: Salary.com, Payscale.com, ZipRecruiter.com, Nurse.org (Check for latest reports)
- Medscape: Annual Nurse Salary Reports (Often require free registration)
- National Council of State Boards of Nursing (NCSBN): www.ncsbn.org (Information on NCLEX and nursing licensure)
Disclaimer: Salary data is subject to change and varies widely by location, experience, and employer. Consult current salary survey data and local job postings for the most accurate information.



