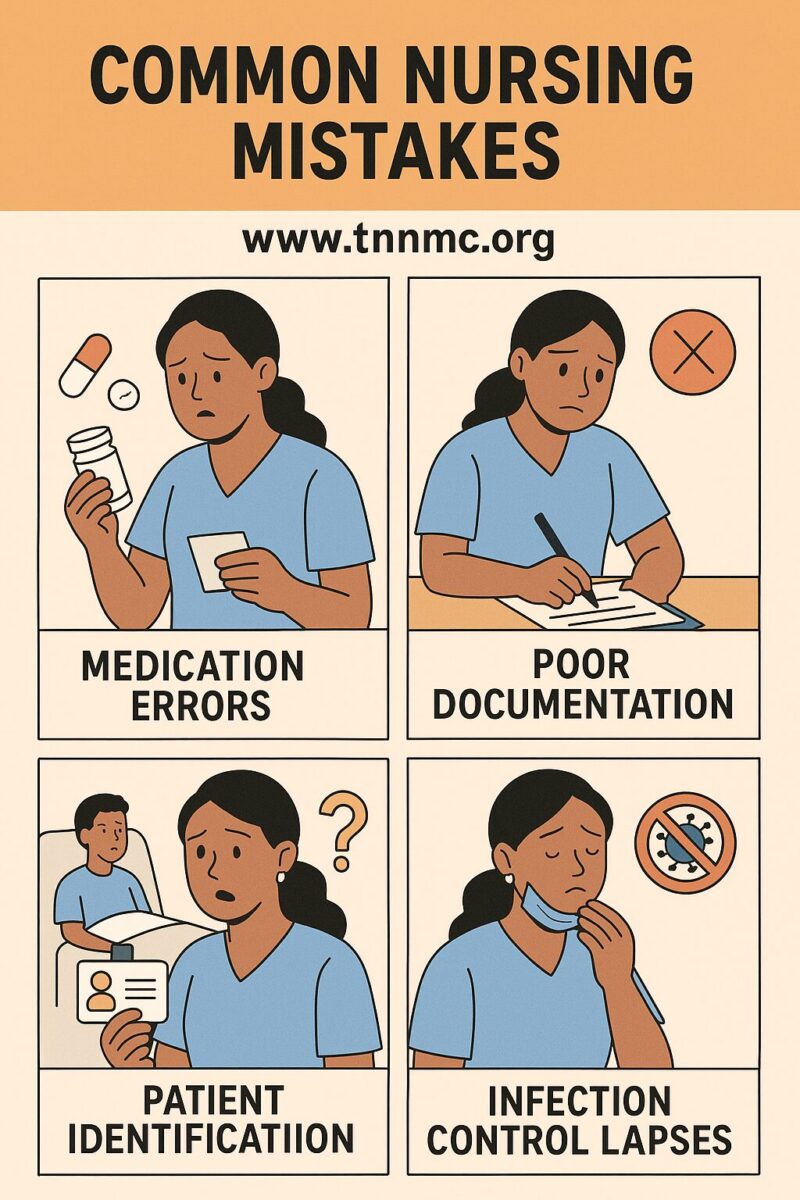
Achieving perfection is practically essential in the medical field, given that healthcare professionals deal with the most precious commodity of all – human life. This is especially true in nursing, where a single oversight can have serious consequences. Yet even the best nurses are human. When you’re just starting out, it’s normal to feel nervous, unfamiliar with the environment, and under intense time pressure – factors that can lead to mistakes. Inexperience, long shifts, heavy workloads, and high-stress situations all contribute to making errors more common. The reality is that mistakes do happen, despite our best intentions. However, by being aware of common pitfalls and taking proactive steps to prevent them, nurses can minimize errors and deliver safe, high-quality care. Below, we discuss several frequent nursing errors and how to avoid them in practice.
Medication Errors
Medication errors are among the most dangerous mistakes in healthcare because they directly affect patient treatments. Administering the wrong medication, giving an incorrect dose, or providing it to the wrong patient are errors that can potentially be fatal. Unfortunately, these errors are alarmingly common; in the United States, medication errors are one of the most frequent medical errors, harming at least 1.5 million people every year. No nurse is immune – whether you’re new or have years of experience, anyone can commit a medication error if not careful.
One major cause of medication mistakes is a lack of presence of mind at the crucial moment of administration. New nurses, in particular, often struggle with nerves, stress, and being rushed, which can lead to lapses in attention. But even veteran nurses might slip when fatigued or distracted. These lapses can result in administering a drug incorrectly, so it’s vital to stay focused. The stakes are high: a simple mix-up in dose or drug can cause serious harm or even death.
How to prevent medication errors? The good news is that most medication errors are preventable by following proper protocols and staying vigilant. Always double-check every step and eliminate distractions when giving meds. Key safety practices include:
- Use patient identifiers: Verify the patient’s identity with at least two identifiers (e.g. name and date of birth) to ensure you have the right person.
- Check for allergies or reactions: Confirm any drug allergies or previous adverse reactions every time before administering a medication.
- Be mindful of diagnoses/conditions: Take note of the patient’s current diagnoses or critical conditions that might affect medication safety (for example, renal impairment, pregnancy, etc.). This context can be crucial in avoiding contraindications.
- Verify current medications: Ensure the patient’s medication list is up-to-date. Knowing all the medications (including over-the-counter drugs and supplements) that a patient is on helps prevent dangerous interactions or duplicate therapy.
- Use accurate measurements: Many dosing errors occur due to inaccurate weight or calculations. Make sure the patient’s weight (and height, if needed) is recorded correctly, as these may be used to calculate doses (especially in pediatrics or weight-based dosing).
In addition to the above, always adhere to the “five rights” of medication administration (right patient, drug, dose, route, time). If something about an order seems off, pause and double-check it or consult a pharmacist/colleague. Taking a moment to clarify an unclear prescription or to recheck a dosage calculation can save a life. By staying mentally present and following these safeguards, you can greatly reduce the risk of a medication error.
Infection Issues
A perioperative nurse performs a surgical hand scrub, illustrating the importance of strict hand hygiene before a procedure. Hospital-acquired infections are a serious patient safety concern in every healthcare setting. According to the CDC, in American hospitals alone, healthcare-associated infections (HAIs) account for about 1.7 million infections and 99,000 associated deaths each year. In other words, on any given day roughly 1 in 31 hospital patients has at least one HAI cdc.gov. These numbers are sobering — they highlight how common and dangerous infections can be if proper precautions are not taken.
Nurses are on the front lines of infection prevention. It is our responsibility to facilitate patient recovery while minimizing complications that could lead to infection. Proper hygiene and aseptic technique are non-negotiable in nursing practice. In fact, many infections stem from lapses in basic infection control practices. Never underestimate the importance of good hand hygiene and cleanliness – iatrogenic infections (those caused by medical care) can result from negligence by healthcare personnel. Something as simple as not washing hands or not using sterile technique when required can introduce harmful pathogens to a vulnerable patient. The upside is that by rigorously following established protocols, most of these infections are preventable.
To protect your patients from infections, always keep the following guidelines in mind:
- Adhere to standard precautions: Treat every patient as potentially infectious. Perform proper hand hygiene before and after any patient contact or procedure – wash with soap and water or use an alcohol-based sanitizer as recommended. Wear gloves, gowns, masks, and eye protection when exposure to bodily fluids is possible. Consistent use of standard precautions is the foundation of infection control.
- Maintain aseptic technique: When performing sterile procedures (such as inserting IV lines, catheters, or dressing wounds), use aseptic technique meticulously. This means keeping equipment sterile, avoiding contamination of sterile fields, and following protocols like the surgical scrub illustrated above. By preventing the introduction of bacteria during invasive procedures, you greatly reduce infection risk.
- Clean and disinfect regularly: Ensure that patient environments and equipment are properly cleaned and disinfected. Wipe down surfaces and high-touch objects (bed rails, IV poles, stethoscopes) with approved disinfectants. Use antiseptics on the patient’s skin for procedures (for example, clean the IV insertion site with chlorhexidine). Regular cleaning breaks the chain of infection by removing pathogens.
- Follow facility infection protocols: Stay up-to-date with your hospital’s infection prevention policies. This includes isolating patients with contagious illnesses as needed (and using appropriate transmission-based precautions like contact or droplet isolation), properly handling and disposing of sharps and biohazard waste, and ensuring vaccinations or screenings (like for MRSA) are done per guidelines. Hospitals have specific protocols to prevent common HAIs (such as catheter-associated infections or surgical site infections) – make sure you know them and comply fully.
By being vigilant and enforcing these infection control practices consistently, nurses can dramatically lower the risk of patients acquiring new infections during their care. Infections may be a constant threat in healthcare, but with good technique and attention to cleanliness, we can keep our patients safe and complication-free.
Documentation Errors
Accurate documentation (charting) is an essential part of nursing – it’s often said, “If it isn’t documented, it wasn’t done.” While hands-on care is critical, so is recording every important detail of that care. In the flurry of a busy shift, it can be tempting to skim over charting or postpone it. However, poor documentation can lead to serious lapses in communication, medical errors, and even legal trouble down the line. Remember that a patient’s chart is a legal record of their care. From a patient safety perspective, other members of the healthcare team rely on your notes to know what has been done and what still needs doing. From a professional standpoint, incomplete or incorrect charts can make you liable for omissions or mistakes if something goes wrong.
New nurses are often surprised by just how much paperwork and electronic documentation comes with the job. It may feel overwhelming at first, but meticulous charting is as important as any clinical skill. Take the time to do it thoroughly. Being aware of common documentation pitfalls – such as forgetting to chart a medication or failing to update a care plan – will help you avoid them and protect both your patient and yourself.
What should you be charting? In short, everything of significance to the patient’s care. Key items that must be documented include:
- Health history and status: Document the patient’s relevant medical history, current diagnoses, and any significant findings on assessment. This provides context for their care.
- Medications administered: Every medication you give should be recorded with the time, dose, route, and any pertinent observations (e.g. patient’s response or any side effects). Also note any discontinued or held medications and the reason (for instance, if a blood pressure medication was held due to low BP).
- Nursing interventions: Record all nursing actions and procedures performed. This could be everything from wound care and catheterizations to patient education and emotional support. If you did it, chart it.
- Changes in condition: If the patient’s status changes (vital signs, level of consciousness, new symptoms, etc.), document what changed, when, and what you did about it. Communication to a physician about the change should be noted as well.
- Physician orders and care plans: Whenever new orders are given (like a new medication, lab test, or therapy), ensure they are noted and that you’ve updated the care plan. Also chart any consultations or discussions with other healthcare professionals regarding the patient’s care.
Thorough documentation creates a clear timeline of the patient’s hospital stay and treatment. It ensures that anyone who reviews the chart (another nurse, a physician, a quality reviewer, or a lawyer in worst-case scenarios) understands exactly what was done and the patient’s progress. If you are ever unsure how or what to document in a certain situation, don’t guess – ask a more experienced nurse or consult your facility’s policies for guidance. It’s far better to seek help than to document incorrectly or leave important information out. By prioritizing accurate charting, you uphold professional standards and contribute to safer patient care.
Calling for Help Without Patient Data
Effective communication is another area where errors can occur. A common mistake (particularly for those new to the role) is calling a physician for help before gathering all the relevant patient information. Imagine needing to report a patient’s worsening condition but not having their latest vital signs, lab results, or medication list on hand when the doctor asks questions – it quickly becomes an awkward situation. Never call for assistance without first getting prepared. This error might not physically harm the patient, but it can damage your credibility and waste valuable time. In the hospital, one of the first lessons is that you should always have the patient’s chart or electronic record in front of you when you contact a physician. Being caught unready (needing to say “I don’t have that information right now”) makes you look unprofessional or “like an amateur” in the eyes of colleagues.
To maintain professionalism and efficiency, do your homework before you call. Assess the patient and jot down key facts. For example, if you’re calling about a patient’s high fever, be ready to report their vital signs, any relevant lab results (like the latest blood counts or cultures), their intake/output, current medications, allergies, and a brief background of the issue. Organize this information (many nurses use the SBAR – Situation, Background, Assessment, Recommendation – format to structure the call). Then call the physician and concisely present the situation with those details at your fingertips. This way, you can answer questions on the spot and get faster orders. By being prepared, you not only get better help for your patient, but you also demonstrate competence. Remember, thorough preparation before calling for help is part of being a responsible patient advocate and a professional nurse.
Patient Falls
Patient falls are a persistent concern in healthcare facilities, and preventing them is a critical nursing responsibility. A fall can happen in an instant and can have devastating consequences for a patient. Often, falls occur when a patient tries to get out of bed or walk without assistance. This frequently happens with those who feel a bit better or are embarrassed to call for help to do something as simple as using the bathroom or fetching a personal item out of reach. Especially at night or after a procedure, a patient might be unsteady on their feet. If they attempt to move around alone and no one is nearby to assist, the risk of an accident is high. Unfortunately, even a seemingly minor tumble can lead to serious injuries – such as a broken hip, a head injury, or internal bleeding – and it can result in significant health setbacks. Beyond the injury to the patient, there are also legal and regulatory implications. Falls in the hospital can be considered preventable “never events,” and they may expose the hospital (and staff involved) to liability or penalties. In short, never underestimate how serious a fall can be. New nurses might not yet have seen the consequences, but experienced nurses know that one bad fall can be life-changing for a patient and career-changing for staff.
The best approach to falls is preventive. Nurses must stay vigilant, especially for patients at high risk of falling (such as the elderly, those on sedatives, post-operative patients, or anyone with mobility or balance issues). Here are some key strategies to prevent patient falls:
- Frequent monitoring: Check on your patients regularly, and increase the frequency for those who are a fall risk. Many hospitals implement hourly rounding – visiting each patient every hour – which has been shown to reduce falls. By keeping a closer eye on at-risk patients, you can address their needs before they feel the urge to get up on their own.
- Ensure needs are within reach: A common reason patients get out of bed is to grab something they can’t reach. Make sure the call bell, water cup, tissues, eyeglasses, phone, and any other personal items a patient might want are easily accessible on their bedside table. Also ensure the bed is in the lowest position and wheels are locked. When everything essential is at arm’s length and the environment is adjusted for safety, patients are less tempted to stand up without help.
- Safe environment: Keep the room free of clutter and tripping hazards. Clean up spills promptly. If the patient needs to walk, ensure they have non-slip socks or proper footwear. Utilize assistive devices (canes, walkers) as appropriate. In some cases, using bed/chair alarms can alert staff if a high-risk patient tries to get up. Make sure any needed mobility aids are within reach as well.
- Encourage asking for help: Perhaps most importantly, tell patients to call for help whenever they want to get up, and reinforce that you want them to ask. Many patients won’t press the call button because they “don’t want to be a bother.” Reassure them that it’s truly no bother – it’s your job and you are happy to assist. Be approachable and patient so they feel comfortable asking. A patient who trusts their nurse and feels cared for is far less likely to take the risk of going it alone.
By consistently implementing these measures, nurses can dramatically reduce the incidence of falls. It requires alertness and a proactive mindset – anticipate that any patient might try to get up, and plan accordingly. When a fall does occur despite precautions, be sure to follow your facility’s protocol: assess the patient thoroughly for injuries, notify the physician and family, document the incident, and reflect on how it might have been prevented to inform future practice. Preventing falls is truly a team effort and a hallmark of good nursing care.
Conclusion:
Nobody becomes a nurse expecting to make mistakes, but recognizing our human limitations is part of maintaining patient safety. By understanding the common errors described above – from medication mix-ups to documentation lapses – and following best practices to prevent them, nurses can uphold the highest standards of care. Vigilance, good habits, and a willingness to learn from errors are key. Whether you’re a newly qualified nurse or a seasoned professional, a commitment to continual improvement and adherence to safety protocols will ensure better outcomes for your patients and a confident, competent practice for you. Remember, even in a high-pressure environment, taking that extra moment to double-check, prepare, or ask for help when needed can make all the difference in delivering safe and excellent nursing care.
Sources:
- NurseJournal. The 5 Most Common Mistakes Made By New Nurses
- PatientCareLink. Healthcare-Acquired Infections (HAIs) – CDC statistics on infection rates.
- CDC HAI Prevalence Survey – 1 in 31 patients has an HAI on any given daycdc.gov.
- Academy of Managed Care Pharmacy (AMCP). Medication Errors – Frequency and cost of medication errors.