Policy Review and Policy Improvement: The Integrated Response to the Nursing Home Crisis (2025).
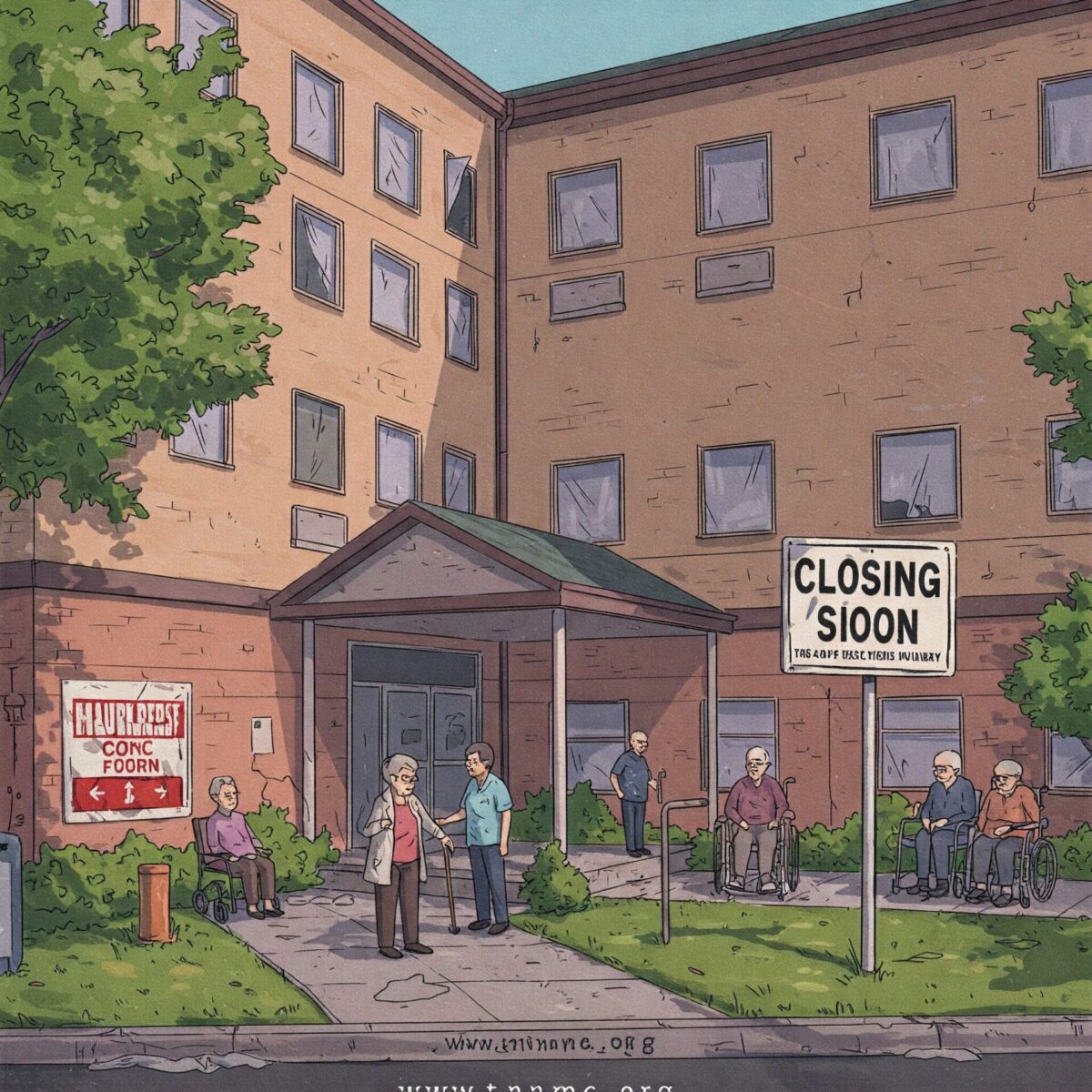
The nursing home sector is in the midst of a multidimensional crisis defined by facility closures, severe staffing shortages and well-documented access barriers. New analysis of existing data shows that 774 nursing homes have shut down since 2020, forcing out more than 28,000 residents, while new openings of facilities have fallen by almost 50% over that time.
And workforce challenges such as burnout — reported among 81% of healthcare professionals — are compounded by inflexible scheduling and a lack of robust support systems. Innovative housing sytems such as the Green House Project or the Netherlands’ Hogeweyk dementia village are discussed as viable solutions, as are technological intervention strategies like AI-assisted monitoring systems.
In light of this fact, this brief summarizes a report that explores potential policy solutions such as flexible staffing models, reimbursement reform, and specialized care pathways to address the growing demands on the long-term care system and ensure its sustainability going forward, all while preserving resident dignity and caregiver wellbeing.
What We Know About Nursing Home Care
The U.S. nursing home industry is facing an unprecedented crisis in 2025, with decline in quality of care for millions of older adults. Ask questions, listen more, and act responsibly in the context of the unique needs of your organization.

Understanding the Crisis: Access, Quality, and Sustainability
The nursing home crisis of 2025 is one mainly of vastly reduced access to care. 46% of nursing homes are limiting new admissions, and 57% have a waiting list of people who want to enter the facility1, according to data gathered by the American Health Care Association and National Center for Assisted Living (AHCA/NCAL). This access is limited despite a rapidly aging population and rising demand for long-term care services.
More evidence of the crisis can be seen in alarming facility closures and capacity reductions. Since 2020, at least 774 nursing homes have shuttered nationwide, displacing 28,421 residents1. The pace of new facility development has also dropped off a cliff, with just 37 new nursing homes opening in 2023 versus 73 in 2020 — a nearly 50% decline1. The first quarter of 2025 shows continuing this trend, with little new capacity coming online even as need increases.
Access issues are joined by concerns about the quality of care. Understaffing has led to 20% of nursing homes closing units, wings, or floors1. This decrease in operating capacity commonly translates into increased patient-to-staff ratios across the remaining units, which can jeopardize quality of care and the safety of residents.
Regulatory Landscape Shifts
There Will be Major Changes to Nursing Home Regulation Again in 2025 Big Changes for Long-Term Care Surveyor Guidance, Effective March 24, 20252 The Centers for Medicare & Medicaid Services (CMS) has issued significant revisions to Long-Term Care Surveyor Guidance. These changes provide for increasing oversight, bolstered compliance expectations and revisions to capstone regulations addressing admission agreements, staff requirements, medication use and quality assurance processes.
A particularly contentious regulatory development is the federal staffing mandate, which the industry says could worsen the access crisis. Without accounting for underlying workforce and funding challenges1, AHCA/NCAL estimates this mandate could lead to displacement of nearly 300,000 residents.
Underlying Factors of the Nursing Home Crisis
Workforce Shortages and Labor Market Dynamics
In 2025, the nursing home industry is still grappling with dire workforce shortages. Nursing homes also lost over 250,000 workers — some 15% of their workforce — during the pandemic — the largest decline in any healthcare workforce10. Unlike other sectors of health care that have mostly recovered, nursing homes still have not returned to pre-pandemic levels of staffing, with a shortfall of more than 100,000 workers persisting into 202519.
The dynamics in the labor market have fundamentally shifted, and healthcare workers are demanding more flexibility as well as control over their schedules. According to a 2025 Healthcare Workforce Trends Survey, 98% of respondents indicated that they have seen an increased demand for flexible, gig-style work arrangements over the last 1-2 years. An additional survey indicated that 67% of healthcare leaders reported increasing burnout and disengagement due to lack of flexibility.
Funding Difficulties and Economic Pressures
There are several threats to nursing homes’ economic viability. Chronic government underfunding through Medicaid—which receives most long-term care residents—has resulted in ongoing financial strain1. This funding gap is compounded by episode and annual record-high inflation and rising operational costs that have outstripped reimbursement adjustments.
Economics of nursing homes have grown more strenuous under Medicare Advantage (MA) plans. Industry observers characterize MA as “tightening the screws” on the industry, including a significant reimbursement gap between Medicare Advantage and traditional Medicare, along with large administrative burdens. These pressures have rendered the business model for nursing homes increasingly unviable, especially for smaller and rural facilities.
Changes in demographics and heightened complexity of care
The basic demographic fact of a graying population leads to an increasing demand for nursing home services. By 2034, for the first time ever in U.S. history, older adults will outnumber children, marking a major inflection point in the healthcare workforce crisis3. For nursing home residents, who have multiple chronic conditions that require specialized care, there is also an increasing clinical complexity of these residents simultaneously with this demographic shift.
High Opening Bid Compensation Needs in Long-Term Care
The Burnout Epidemic Plaguing Nursing Homes
In 2025, there is a looming burn-out crisis in the nursing home workforce. A recent systematic survey of health care workers found that 81% report burnout, with 62% currently burned out and 49% considering leaving the profession altogether3. Such professional exhaustion threatens the very bedrock of workforce stability, as well as the quality of care our residents receive.
Burnout is multidimensional and has 3 key components: emotional exhaustion, depersonalization (the turning of one’s attitudes toward residents into detached forms), and diminished personal accomplishment17. These symptoms fully correlate with turnover intention, forming a self-perpetuating cycle of staffing instability.
Indeed, only 24% of nursing personnel from a global sample of over 9,000 nurses in 35 countries reported that their institutions offered sufficient mental health services20. Based on those data points, many employers offer little more than self-care methods that, although beneficial in individual contexts, will not eradicate the messy structures of workplace stress.
The Flexibility Imperative
Flipsides of rigid scheduling have become key drivers of workforce dissatisfaction and turnovers. An analysis of healthcare professionals who had paused their careers revealed that 78 per cent identified flexibility and control over when (and if) they worked as the key component driving consideration of returning to the workforce3. That longing for independence has turned into not just a wish but an entitlement among health-care workers.
The 2025 Healthcare Workforce Trends Survey corroborates this trajectory, noting flexibility as the number one most important factor for most nurses in workforce decisions (78% of the respondents)14. 40% of healthcare leaders believe that more than 50% of their nurses would benefit from working on flexible schedules14. This is a sea change in workforce expectations that nursing homes need to adapt to in order to be competitive employers.
Barriers to Upward Mobility
The nursing home industry is facing issues of recruitment and retention. Inadequate opportunities to advance your career and develop your knowledge can lead to poor retention. A lot of facilities in the elder services industry do not have structured pathways for progress, which can make their staff feel undervalued and unmotivated to do their jobs.
Moreover, limited training focused on specialist geriatric care leads to deficiencies in clinical competence. As resident acuity grows, staff are often lacking specialized skills to help residents with complex diseases such as dementia, multiple chronic illnesses and end-of-life care. This disconnect hinders the opportunity for a personalized, needs-driven care approach and creates stress for caregivers that can lead to compromised care quality.
Analysis of Policy: Current Policy Frameworks and Global Perspectives
Recent CMS Regulatory Changes
In 2025, there are major policy changes being enacted by the Centers for Medicare & Medicaid Services that will change how nursing homes operate and how they are overseen. Scheduled to be in effect on March 24, 2025, the new Long-Term Care Surveyor Guidance makes a few fundamental changes 2:
The re-enforcement of agreed standards for admission and ensuring these do not contain terms which require third-party payment guarantees
Expanded oversight on transfers and discharges, with guidance on resident transfer rights
Enhanced staffing enforcement utilizing PBJ data as the main measure
Stricter rules around psychotropic medication use, including bans on using it to sedate residents for staff’s convenience
Quality assurance and performance improvement requirements, including for health equity considerations2
CMS has also updated its Nursing Home Care Compare website and Five Star Quality Rating System methodology to account for false positive schizophrenia coding as well as to remove citations in dispute16. These changes seek to boost transparency and accountability but add administrative complexity for providers.
Federal Hiring Mandate Controversy
One of the most contentious policy issues in 2025 is the implementation of federal staffing mandates. AHCA/NCAL has stated that the staffing mandate, imposed in the absence of commensurate funding increases, will exacerbate the access crisis and could lead to the eviction of 300,000 residents of our facilities1.
Industry advocates say that while staffing standards matter for providing quality care, imposing them against a backdrop of dire workforce shortages and insufficient reimbursement creates a lose-lose scenario for many facilities. They say the mandate treats symptoms, not core causes of staffing problems.
Policies for Eldercare in Scandinavia
Scandinavian countries offer instructive policy alternatives emphasizing the public provision of eldercare. From 1993 onwards in Sweden, and from 2000 to 2014 in Norway and Denmark, laws were introduced which further strengthened legal rights to publicly provided care services9. All three countries had developed some form of legal guarantees for social care services for older adults by 2014.
The Scandinavian model relies on large-scale public investment in eldercare and an emphasis on independence and dignity. However, even those systems struggle with challenges relating to workforce recruitment and retention. How to best combine work and family rather than have the choice between the two currently remains for many a choice they have to make within the context of very few genuine work-family facilitating measures for family caregivers8.
Innovative Care Models
The Green House Project
The Green House Project is an innovative model of long-term care that transforms the design and operation of nursing homes. This model establishes small homes that house 10-12 residents, with private bedrooms and bathrooms enclosing shared spaces for the community such as a hearth area, kitchen, dining room, and outdoor gardens6.
The Green House model turns traditional nursing home hierarchies on their head. Nursing assistants, referred to by the home as Shahbazim, dutifully partner with nurses and therapists to manage residents’ care—inverting the traditional hierarchy of organizational structure6. Empowering direct care staff improves job satisfaction and leads to more customized resident care.
Research indicates this model yields important improvements in resident outcomes. Research from the Robert Wood Johnson Foundation found that the Green House residents are “happier and healthier” than people in typical nursing homes6. Emphasis on authentic home experience instead of institutional experience reinforces resident dignity and independence.
The Dementia Village: Hogeweyk
Hogeweyk, an enclosed model village in Weesp, Netherlands, has created a new paradigm of care for people with dementia. This state-of-the-art facility provides an immersive environment tailored to older adults affected by dementia, including a town square, supermarket, hairdressing salon, theater, pub, and café-restaurant, plus twenty-seven homes modeled in various living styles that mirror their pre-dementia lives7.
The village design enables people to follow familiar daily routines in a safe, controlled setting. Staff members wear regular clothing rather than clinical attire, taking on roles that are tailored to the social context of each housing unit. With less reliance on medication and higher levels of activity than residents at traditional nursing homes7, this holistic approach to reminiscence therapy has proven to be extremely beneficial.
Its success suggests that environmental design and operational philosophy can vastly enhance patients’ quality of life, while also potentially reducing medication costs and staff turnover.
Sweden’s Esther Model
Another innovative approach is Sweden’s Esther Model, pending evaluation, which is focused on improving care coordination for elderly patients with complicated needs. Created in Jönköping County, the model solves the problem of siloed care typically seen when older patients receive care from multiple specialists, primary care physicians, emergency departments, hospitals, and long-term care providers4.
This model introduces a symbolic patient — “Esther” — which helps organizations keep the patient experience front and center through transition of care. This patient-centred model overcomes the silos between hospital, physician, and community care services, which are funded and provided by different entities, as mandated by Swedish law4.
The Esther Model enhances patient-centered care by structuring it around the patient journey rather than policy and organizational silos, thereby reducing the number of unnecessary transitions and interruptions in care, as well as potentially reducing hospitalizations.

Emerging Technological Solutions for Eldercare
AI and Robotics Applications
AI and robotics are promising technologies that can be used to address a number of key problems in eldercare. The use of AI algorithms have the potential to transform health monitoring by analyzing data from wearable devices and electronic health records, providing real-time analysis, detecting the early warning signs of diseases, and developing personalized treatment recommendations5.
Examples of AI applications in nursing homes involve diagnostic and management algorithms, virtual medical consultations, and refined assessment of conditions such as osteoporosis, including fracture risk assessment accounting for age, frailty, and life expectancy5. These technologies could help expand clinical capacity and ease the burden on staff.
It means — Robotics are complementary to AI-based systems and serve the purposes of physical assistance and companionship. Assistive robots can support mobility, medication management, and activity of daily living, extending the length of independence for older adults while alleviating the burden on caregivers5. Social robots tackle isolation and loneliness, offering interaction and cognitive stimulation for residents.
Online Medical Advice and Monitoring
Telehealth implementation in nursing home care has been expedited, allowing for remote monitoring and virtual consultations that enhance the availability of specialist care. AI-enabled telemedicine platforms permit continuous monitoring of vital signs and vulnerability local for health deterioration, and particularly benefit those facilities located in remote or underserved areas5.
These technologies improve clinical oversight and decrease avoidable transfers to the ED. Residents with chronic conditions requiring specialist management can access expertise in timely care through telehealth consultations without the stress and risks of facility transfers.
The Ethical Dimensions of Nursing Home Care
Ethics of Resource Allocation and Staffing
Ethical dilemmas of resource allocation permeate nursing home operations. In a national survey of nursing home staff, 79% named lack of resources as their number one ethical challenge8. This scarcity leads to daily moral distress for caregivers who face challenging prioritization decisions that could undermine the quality of care.
Staffing shortages magnify these ethical quandaries, making it so that difficult decisions must be made about which residents’ needs can be addressed immediately and which will have to wait. The chasm between resident needs and available staff leads to a persistent source of moral injury to caregivers who “know” what constitutes ideal care and know what they can pragmatically deliver.
End-of-Life Care and Autonomy
End-of-life issues are the second most frequently reported (39%)9 ethical challenge reported by nursing home staff. These challenges include decisions regarding life-prolonging treatments, palliative care approaches and balancing resident preferences with family expectations.
Records of ethics meetings in nursing homes document that decisions regarding end-of-life care often take up much of the case discussion8. Notably, while family members are often included in such ethics meetings, the residents themselves often are not — making it an ethical dilemma of autonomy and voice when it comes to decisions about critical care.
Coercion and Resident Rights
Coercion was reported as the third most common ethical challenge raised among nursing home staff (33 %)8. This includes concern for the use of restraints, whether physical, chemical via psychotropic medications, or restraints on resident movement or choices.
Recent guidance from CMS specifically addresses chemical restraints, bringing oversight of psychotropic medications under regulations prohibiting their unnecessary usage2. The guidance prohibits the use of medications to sedate residents for the convenience of staff, and requires explicit consent for the initiation or increase of psychotropic medication2
Recommendations
Workforce Solutions
Adopt Flexible Staffing Models
Flexibility should be a core workforce strategy for healthcare organizations rather than an occasional accommodation. To help compete in a changing labor market14, facilities can develop internal pools of resources, create part-time options with benefits, and implement self-scheduling systems.
Evidence indicates that flexibility is the chief incentive for 78% of healthcare professionals to come back3 or stay in the workforce. Those facilities that shift their staffing models to accommodate this preference will have a competitive advantage in recruitment and retention.
How to do it: Develop Comprehensive Mental Health Support
Facilities need to develop strong mental health support systems for staff, rather than simply suggesting self care, but creating programs. Recommendations include:
Counseling services available on-site with convenient scheduling
Trained facilitators conducting peer support programs
Political ideology affecting which seals get the bread crumbs
Leadership training on how to recognize and deal with burnout
Set Clear Succession Planning Steps
Career ladders with defined structures and accompanying increases in compensation give staff members a roadmap of growth potential. Programs should include:
Specific clinical tracks (wound care, palliative care, dementia care)
Mentorship components in leadership development programs
Aggressive tuition assistance for graduate education
Programs that rightly reward expertise and contribution
Policy and Funding Reforms
System Overhaul of Medicaid Reimbursement
States could adopt value-based Medicaid reimbursement models that take into account resident acuity, quality outcomes, and regional cost differences. Payment rates need to be based on the actual costs of delivering care, including competitive wages for employees, not arbitrary budget caps.
Set up loan forgiveness programs
Federal and state governments need to enhance loan forgiveness programs for nursing home jobs. There would be incremental forgiveness available based on years served, and significantly accelerated forgiveness tied to work in underserved areas or facilities with documented staffing challenges.
Establish Regulatory Alignment and Reduction Initiative
Federal agencies should conduct a broader regulatory review to identify conflicting or duplicative requirements that add administrative burden without enhancing residents’ outcomes. Reducing the amount of documentation required would free up staff to spend more time directly with residents.
Care Model Innovations
Scale the Green House Model
State Medicaid programs should provide financial incentives for converting existing traditional nursing homes to Green House or similar small-house models. This could include:
Renovation-capital-improve-grant
Increased reimbursement rates for small-house models that have documented better outcomes
Technical assistance programming to aid conversion planning and implementation
Develop Specialized Dementia Care Pathways
Extensive supportive environments for patients with dementia should be modeled on Hogeweyk, allowing them to maintain stated social customs, support and minimize medications. Design 1: Elements of the design should include:
Circular pathways that offer safe exploration
Landmark Features and Environmental Orientation Cues
Stations that inspire interaction with familiar activities
Training of all staff in communications skills specific to dementia
Develop Integrated Care Coordination Systems
Nursing homes should adopt formal care coordination protocols with hospitals, primary care practices, and specialty providers, following the model created in Sweden by Esther. This should include:
Coalesced electronic health records with pertinent clinical data
Identified transitions coordinators tasked with managing transitions
Periodic case conferences with all stakeholders across the care continuum
Standardized communication tools for transfers between settings
Technology Integration
Integrate AI into Monitoring Systems
Having AI-driven monitoring systems on campus that can pick up on subtle changes in resident condition before clinical deterioration is apparent. These systems should:
Use data from wearables, EHRs and staff observations
They can train on data until the end of October 2023
Enhance clinical decision making, without replacing human judgment
Use appropriate data protocols that respect privacy
Create Standards for Telehealth Integration
Best practice standards: Industry associations should develop best practice standards regarding the integration of telehealth in nursing homes that address:
Connectivity: technical requirements for reliable τoτ connectivity
Clinical workflows that optimize a given telehealth modality
Templates in documentation for virtual consultations
Staff training requirements for facilitation of telehealth visits
Conclusion
But the nursing home crisis of 2025 is an unprecedented challenge — and even more so, an opportunity for bold, out-of-the-box solutions. What happens when a shortage of workforce and economic pressures and increasing care needs amid regulatory changes come together at the same time? A perfect storm that could threaten access to long term care services for the nation’s most vulnerable elderly.
This analysis will illuminate both the nature of the current crisis and hopeful paths forward. Facility closures, admissions ceilings, and staffing challenges are symptoms of a systemic malaise that can’t be solved with piecemeal interventions. Instead, the challenge is one of systemic reform across workforce development, funding mechanisms, care models, and regulatory frameworks.
The workforce crisis requires specific consideration, with nursing home staff members plummeting to never-before-seen levels of burnout and expectations shifting around how much flexibility (and support) the workplace should give. Groups that embrace these new workforce realities — with flexible scheduling, mental health support, and clear advancement pathways — will enjoy a competitive edge in recruitment and retention.
Among these, the Green House Project’s small-home model, Hogeweyk’s dementia village model and Sweden’s Esther Model for care coordination would be particularly beneficial if adapted to international partners. These innovations show that radically different ways of caring for elders are not only possible, but result in demonstrable improvements in residents’ and staff members’ wellbeing.
Recent advances
Recent advances in technology, especially AI-powered monitoring, as well as the integration of telehealth, provide a path to improve clinical capabilities, and potentially reduce the burden on clinical staff. But tech should augment, not displace, the human connections that are the core of quality care.
The ethical aspects of nursing home care — especially around resource allocation, end-of-life decision making, and resident autonomy — do not require institutional safeguards but more sophisticated systems to provide staff with the tools they need to navigate complex situations.
Ultimately, fighting the nursing home crisis means understanding the inherent meaning of eldercare in our society. Sustainable solutions require adequate funding, innovative models and a change in culture that recognizes the dignity of residents — and of their caregivers. To put this system in place we must act — together — as policymakers, providers, workforce participants, and advocates to create a long-term care system that works for those who are aging.